Winter Foot Care for People with Diabetes
Stephen Taylor
Deputy Head of Podiatry /MPTT
Isle of Wight NHS Trust
Autumn is here again: the swallows have flown south, the leaves are already beginning to fall and the nights are drawing in. But there is still much to look forward to: frosty mornings, the bright winter constellations, the festive season and even the possibility of snow. This article follows our Head of Department – Steph Stanley’s article “Summer Foot Care.” Steph’s article discussed summer foot problems like: sunburns, dry heels, foot fungus, barefoot walking injuries etc. The changing of the seasons and coming of the cold weather presents new problems for people with diabetes. This is particularly true for people with diabetes who have reduced circulation to their feet (peripheral vascular disease) or nerve damage (peripheral neuropathy) in their feet.
In colder weather people return to wearing closed in shoes. Shoes can protect neuropathic feet from injuries, but if the toe-box of the shoe is too narrow or shallow then corns and callous can form around the bony prominences of the toes. Corns and callous can become the focal points for ulcers to develop especially in neuropathic feet. When choosing shoes you should have your feet measured and shoes properly fitted (especially if you have neuropathy). Day shoes should be flat with a broad, deep toe box. They should have laces, buckles or velcro straps. Soft leather is preferable to prevent rubbing of the toes or blister formation. Shoes should not be too tight or too loose and if you suffer from neuropathy it is advisable to break in new shoes carefully.(2,3,4)
The Diagram below shows a shoe which is too narrow for a person’s foot. Corns/callous will often form around the toes when shoes are too narrow.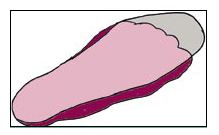
Winter also brings more wet and slippery conditions. This can be a particular problem for people with diabetes who have neuropathy. Neuropathy can make it difficult to properly feel the ground they are walking on. Elderly people are also often more unsteady when walking due to frailty and balance issues. Sometimes people with neuropathy will say it feels like walking on bubble wrap or a board. This may cause slips and trips injuries. To prevent this it is advisable to avoid high heels, especially if the heels of the shoes are narrow. If you are unsteady when walking, a walking stick (or two) can be used to increase your base of gait and make you more stable. Taking shorter strides in slippery conditions can also prevent falls. If you are concerned about falling, you can contact your GP for a falls review.
Cold weather can also cause chilblains, particularly in feet with peripheral vascular disease. When your skin gets cold, the small blood vessels, just below the skin surface narrow. The body does this to maintain its core temperature. Less blood and oxygen flows to the skin cells, but the skin cells are cold and their metabolism is slow, so the cells do not miss the oxygen. As result of this our skin looks pale in cold weather. When our skin warms up the cell metabolism speeds up again and the small blood vessels widen and the blood flow increases again. However, in people with chilblains the blood flow does not increase quickly enough to meet the needs of the skins metabolism and blue/red blotches appear on the skin especially around the tips of the toes, particularly if the person tries to warm their feet up to quickly. You should avoid warming your feet up too quickly (e.g. pu????ing your feet on a radiator or hot water bo????le) especially if your circulation is weak. People with neuropathy also need to be careful not to burn their feet. Bathwater temperature should be checked using the person’s elbow or a thermometer (45oC). If you are susceptible to chilblains you should always wear warm socks (or two layers of socks) in cold weather. You should also make sure your footwear has enough space to accommodate the extra thickness of your socks allowing space to wiggle your toes in the toe-box of your shoes. Chilblains can also be treated by rubefacient creams from the chemist (creams to increase in blood circulation) e.g. creams that contain oil of wintergreen or menthol.(5,6,7)
In 2008 the mountaineer Alan Hinkes gave a talk on the Isle of Wight. He had climbed the 14 highest mountains in the Himalayas and endured extremely cold conditions on all of them. He began his talk by showing off his toes. Unlike many of his fellow climbers he had never suffered from frostbite. He spoke of the importance of good nutrition and particularly hydration (in his case hot cups of tea). He also discussed the importance of hydration in his book (2013) – “Dehydration can be a killer. At altitude it can cause your blood to become more viscous, which can lead to thrombosis and even death. A cup of tea could be a lifesaver.” 8 Alan’s advice complements the NHS advice to people who are susceptible to the cold (e.g. children, elderly, heavy drinkers and drug users). When outdoors you should stay warm by: planning the activity in advance, dressing for the weather conditions, bringing extra layers in case the weather gets colder, not being far from help and having warm non-alcoholic drinks.(8,9)
In conclusion I would finish with a quote from Steph Stanley’s “Summer Foot Care” article. “Over 100 amputations are carried out every week on people with diabetes because of complications connected with their condition. Up to 80 per cent of these are preventable”. Whatever the season there are some basic foot care tips that people with diabetes should follow to avoid injuries and ulcers.(10)
- If you cut your own nails, cut them straight across and file them to the shape of the toe.
- Don’t walk barefoot.
- Check your feet daily.
- Dry skin on the feet (especially the heels) can be treated with moisturiser cream.
- If you develop an open wound/ulcer on your foot, cover it with a sterile dressing and contact Podiatry as soon as possible.
Isle of Wight NHS Trust Podiatry services operate Monday to Friday. The service is provided at the community clinics on the next page. For an emergency appointment please telephone at 9.00am or contact the Podiatry Department at St. Mary’s Hospital.
St. Mary’s Hospital Clinic – 534933
Ryde Health Clinic – 618444
Arthur Webster Clinic (Shanklin) – 862367
Cowes Health Clinic – 290583 or 290979
Brookside Clinic (Freshwater) – 534933
East Cowes Health Clinic – 552532
On weekends please contact: Accident and Emergency.
(1) https://www.thedailybeast.com/could-hygge-help-cure-your-trump-anxiety-the-calming-lifestyle-trends-for-2017
(2 )Marcovitch K, Black’s Medical Dictionary 42nd Edition. London: A & C Black Publishers Ltd 2010: 103 & 120
(3) https://bnf.nice.org.uk/treatment-summary/warts-and-calluses.html
(4) https://www.nhs.uk/conditions/corns-and-calluses/
(5) Sharma R, Then Element Family Encyclopaedia of Health Shaftesbury. Dorset: Element 1999: 128
(6) https://cks.nice.org.uk/chilblains
(7) https://www.nhs.uk/conditions/chilblains
(8) Hinks A. (2013) 8000 meters Climbing the Worlds Highest Mountains Cumbria
(9) https://www.nhs.uk/conditions/Hypothermia
(10) N. Holman & R. J. Young & W. J. Jeffcoate, Variation in the recorded incidence of amputation of the lower limb in England, Diabetologia: 2012 55:1919–1925.
